*Editors note: CGH has responded to the incident, we have placed a link to their statement at the end of the article*
Hospital stays are always jarring for everyone involved.
It is a new environment with a loved one that might not be in the best of health.
That's why hospital staff play a huge part in easing these worries, and perhaps provide some peace of mind, and general care, for those involved.
One Singaporean felt that care was missing during her grandmother's stay in Changi General Hospital (CGH)
Not enough
Isabella Lim took to Instagram to air her frustrations with what she considered inadequate care by CGH.
The crux of her problems were on how her grandmother had developed bedsores, which are areas of damaged skin and tissue caused by reduced blood circulation to vulnerable areas of the body.
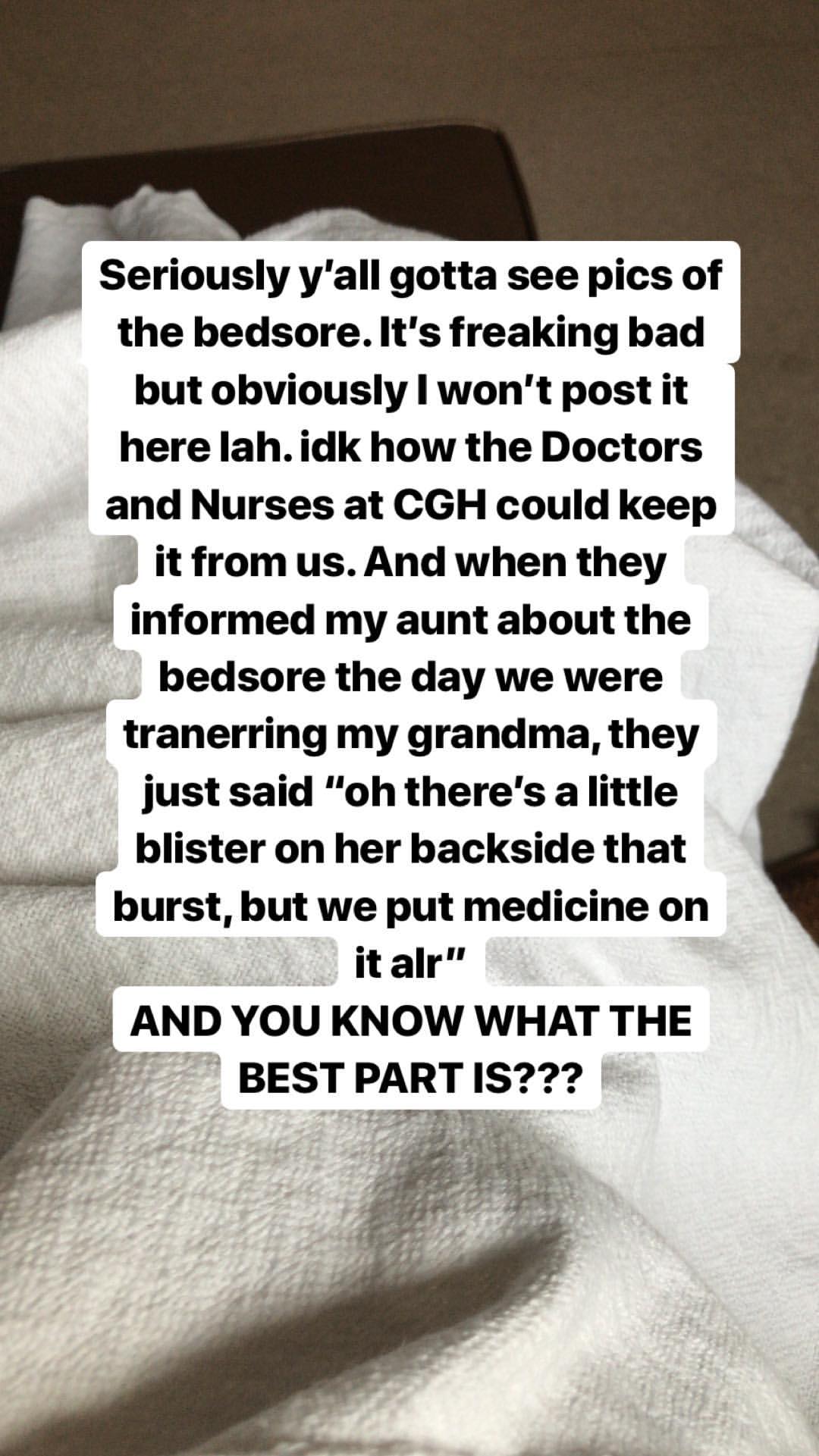 Image from Pretty Wild Things Instagram
Image from Pretty Wild Things Instagram
But Lim's issue with CGH wasn't just limited to the bedsores.
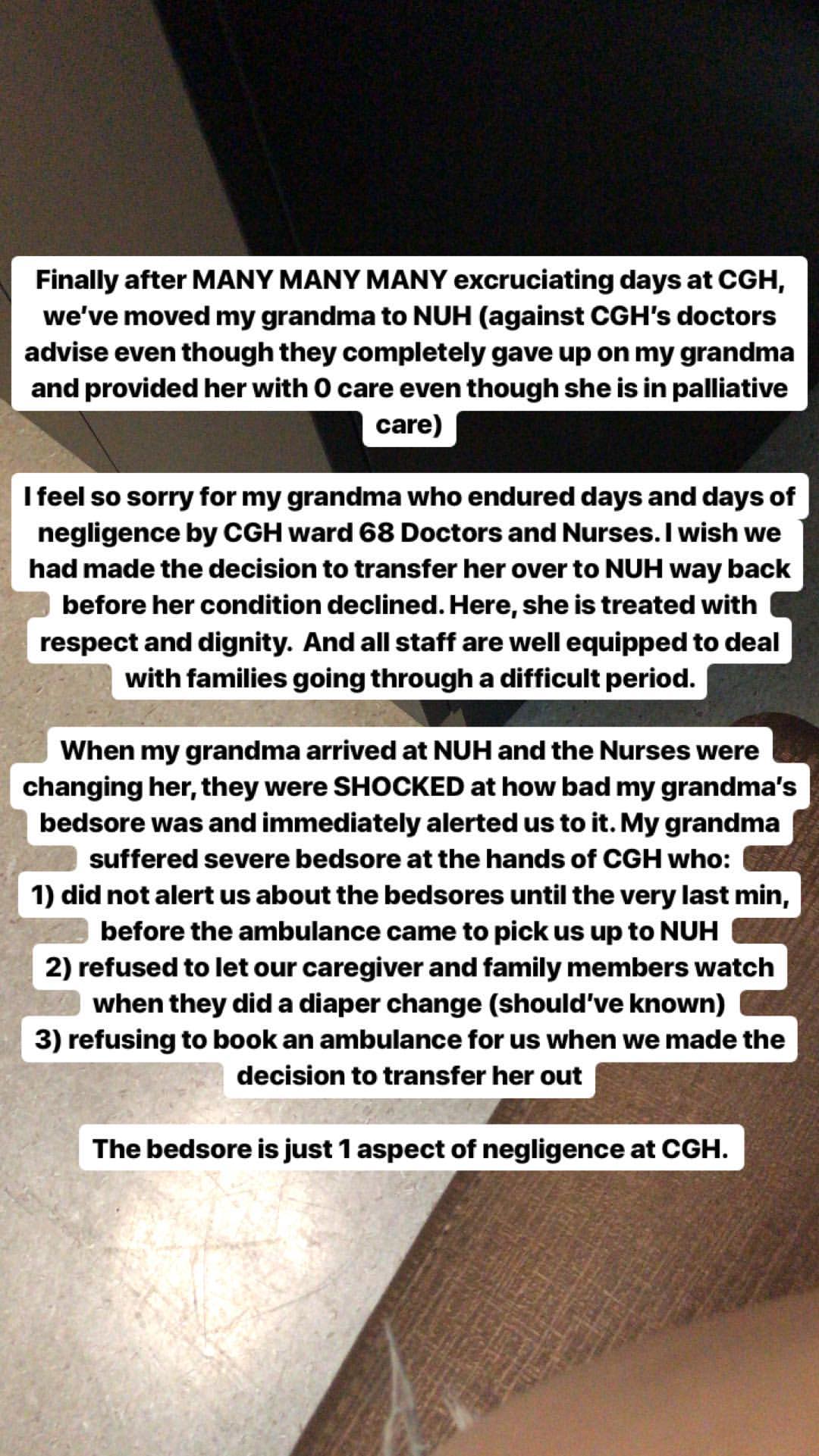 Image from Pretty Wild Things Instagram
Image from Pretty Wild Things Instagram
Most of it had to with what she felt was a lack of accountability in informing the family of their grandmother's condition.
In a Facebook post on May 13, 2019, she expanded on her problems with CGH.
In detail
Here's a rough timeline of what happened.
On Feb. 19, Lim's grandmother was admitted to CGH due to a fall at home, which resulted in a compression fracture.
Unfortunately, while in CGH, her dementia worsened, which eventually resulted in her being admitted to the dementia ward.
Not only that, she contracted Urinary Tract Infection (UTI) during her stay, but was discharged after it cleared.
The respite was brief though, and she was once again admitted to CGH on April 7.
By April 18, she was transferred to the dementia ward, Ward 68.
There were to be more devastating news within the next few days.
The doctors suspected that Lim's grandmother had ischemic bowel, although surgery was deemed impossible due to her condition.
This led to the aforementioned palliative care, which basically meant they were treating this as a terminal case.
On April 25, the family was told that the elderly woman would only have a few days to live.
From April 26 to May 3, Lim was at the ward from 9am till 2am, which allowed her to witness what she thought was inadequate care towards her grandmother.
"During the days that I was at CGH ward 68 every day from morning 9am till 2am at night, I saw how some of the nurses and doctors were unprofessional, unsympathetic and insensitive towards my grandma and family."
Lim listed out some of the issues she had with the staff.
1. Family members not updated with complete information
Lim claimed that CGH staff administered morphine to her grandmother, without informing the family about it.
They only came to know about it after seeing the change from her being fully conscious, to being "super unresponsive".
Lim considered it even more destressing due to the fact that her grandmother, who couldn't speak/ understand English and was suffering from dementia, probably wouldn't have the agency to decide if she wanted the morphine.
2. Unsympathetic, insensitive and unprofessional staff
Lim had quite a few examples under this header.
Despite the doctor's recommendation of a heater blanket to keep her grandmother warm, Lim realised the blanket was missing one day.
When she asked the nurse where it went, this is what the nurse apparently told her: “Put everyday got cost you know??”
They in fact did not know, as the family was apparently not privy to this additional cost, nevertheless, they opted to continue using the heater blanket.
Other issues included how the on-call doctor did not know about her grandmother's condition, rude behaviour from the doctor and nurses, and how on-duty personnel were seemingly unperturbed by her grandmother's heart rate going from 40bpm to 110bmp.
Their response to questions about the heart rate yielding an "it depends on God" also frustrated Lim.
3. Refusal of blood test
Another of Lim's problem with the care was how they declined to give her grandmother a blood test, despite an apparent stabilisation of her condition.
"We spoke to the doctors about this and were denied the blood tests because according to them, “the results will be the same, so no point doing another blood test”."
Here's the difference she found in NUH's treatment of the matter.
"On 3rd May, the day we transferred my grandma to NUH, they finally agreed to the blood test and we actually found an improvement in her lactate count and WBC count, however, by then her kidneys had already started to shut down. If the blood test had been done earlier when we requested for it, would it have been different? Maybe. Maybe not. But we wouldn’t know because they refused to do it."
5. Poorly run wards
Her final gripe involved what she considered a shortage of manpower, or an inadequate usage of existing manpower.
"The nurses were not present at the nurse station or the ward most of the time. We always had to wait, had to request for change of diapers, change of position to avoid bedsores etc.
there was almost no initiative taken by nurses and most of the time, our family members did everything. We even helped open the doors to the ward (ward 68 is locked and requires a button to open the door) because there was no one available at the reception desk to do so and the doorbell would RING for ages until someone opened the door."
NUH change
All those reasons prompted the family to change hospitals, not for some hope or miracle, but just to ensure the grandmother would be given proper care in her final days.
Which appears to have been the case.
"When she was admitted, the nurses alerted us to my grandma’s severe bedsores. The bedsores were really bad. We knew the bed she was using at CGH helped prevent bedsores but we had NO IDEA that her bed sores were this severe.
NUH immediately started treating the bedsores by applying creams and protecting the wound with medicated gauze - something CGH did not do. They also moved my grandma every 1-2 hours. At CGH, the nurses never moved her until they were changing her diapers, so we always had to do so ourselves."
This was a change Lim really appreciated.
"The service at NUH from the moment we reached the hospital was a complete change from CGH. My grandma was immediately placed under end-of-life care and we were given booklets and guides on how to cope with end of life.
My grandma was given heel sponges to prevent further bedsores and compression stockings for her severe water retention - none of which were done by CGH. They conducted frequent checks (diaper change, position change) on my grandma every 1-3 hours. Also, before they did anything to my grandma, they would say “Ah ma, sorry ah, I’m going to change your diapers” compared to some of the CGH nurses who could still joke and laugh with each other while they were changing her diapers.
The doctors and nurses at NUH are better equipped to deal with families going through a difficult time. They were kind, sensitive and respectful to my grandma (and us) and it felt like they were giving her 100% care even though she was going to pass.
They also moved us to a private room. The last 3 days of my grandma’s life at NUH was made so much better. She was comfortable and she was treated with respect and dignity, like any other normal patient in the hospital would be."
Here's the thing though: Lim claims to have faced an issue even trying to get her moved from CGH to NUH.
"My family considered a transfer to NUH many times. Whenever we brought it up to the doctors, they would deny our request stating that “doctors in the other hospital would say the same thing” or “she would probably die on the way in the ambulance” so there was no point."
Other questions involving care were raised by Lim.
"We had a talk with the primary care doctors and they reiterated that my grandma was on palliative care and they were giving her the best they could. Were they? Were they trying to maximise the quality of life of my grandma during her last days or were they just waiting for her to die???"
In conclusion, Lim had a request for hospitals.
"To be honest, it really felt like the staff at CGH had given up completely on my grandma when they decided to put her under palliative care. Just because she was on palliative care, does it mean that a hospital doesn’t treat her bedsores? Does it mean that they can give her as little care as possible? No. You treat a dying person with the same dignity and respect as you would treat a regular patient."
Some advice for CGH.
"CGH, I urge you to re-evaluate your training towards your staff for end-of-life protocols! Learn how to deal with families who are going through a difficult time. Don’t make insensitive remarks like “it depends on God”. Most importantly, treat your dying patients with the same respect and care you would give to a regular patient in the hospital. It was heartbreaking to see my grandma in the state that she was during the last days of her life. In fact, I wish we had admitted her to NUH from the start. Now, we have to pay a 5 figure medical bill to CGH for what? Disappointing service."
And sincere gratitude to NUH.
"My grandma passed away peacefully on 5th May 2019 in NUH surrounded by all her children and grandchildren. My family would like to thank the doctors and nurses at NUH Ward 6A for making the last 3 days of her life a much more comfortable one. Thank you all."
We have reached out to CGH for comment.
CGH's statement
Image collated from Isabella's Instagram
Content that keeps Mothership.sg going
??
Here's how not to get fat while stuffing your face with Hello Pandas.
?? ?
You think it's easy to be a father? This guy has something to say.
???
Remember when you had to practice ting xie (Chinese spelling) like there was no tomorrow?
?️?
You probably know "Speak of Cao Cao, and Cao Cao arrives". But did you know he sometimes arrives in a Gundam suit?
??
Maybe can steam fish with this and make gr8 ginger recipes.
If you like what you read, follow us on Facebook, Instagram, Twitter and Telegram to get the latest updates.