Mass infrared fever screening devices are so common everywhere these days at airports, hospitals and shopping malls, you wouldn't bat an eye when you bump into one.
But not many are aware that Singapore created the world’s first infrared-based mass temperature screening system back in 2003, when the Severe Acute Respiratory Syndrome (SARS) hit Singapore.
The system was subsequently named by Time as one of the best inventions of 2003.
Most incredibly, the idea was quickly turned into a usable prototype within a week in Singapore -- a testament to the remarkable pace the various state institutions had to work at in collaboration with one another.
After putting many heads together, what resulted was the first thermal-imager-based system in the world to be used solely for mass human temperature screening and is now deployed worldwide.
Singapore needed a mass temperature screening solution fast
On March 1, 2003, Patient No. 1 was admitted to Tan Tock Seng Hospital for a suspected case of pneumonia.
The ailment was christened SARS two weeks later.
By March 24, 2003, the Infectious Diseases Act was invoked.
There was a need overnight to efficiently screen large groups of people for fever as it was the only known symptom of SARS.
The World Health Organisation (WHO) and Communicable Disease Centre (CDC) guidelines stated that a suspect case was one whose body temperature is greater than 38°C.
This was especially critical at immigration checkpoints to control the spread of the disease.
A system was needed fast to screen large groups of people quickly, non-intrusively, and with a high level of confidence in sieving out febrile persons.
Febrile persons are people having or showing the symptoms of a fever.
Literally overnight, a new screening device was created in Singapore without generating too many false positives and false negatives.

First mass screening prototype
On April 3, 2003, slightly more than a month after SARS struck, the Singapore Ministry of Health approached the Defence Science and Technology Agency (DSTA) for possible alternative solutions to screen temperatures of a group of people quickly.
DSTA manages complex defence science and technology programmes and conducts research and development (R&D) in multi-disciplinary areas.
Working with MOH to understand the requirements, DSTA quickly came up with a design concept using the Singapore Armed Force's existing military thermal imager.
Singapore Technologies (ST) Electronics, which designs and manufactures thermal imagers, was roped in to work together in this project.
A trial was conducted at the Accidents & Emergency Department of Singapore General Hospital on April 4, 2003 -- a day later.
The system was tested on febrile individuals to ensured that it worked.
Despite the small sample size of seven high fever patients present for the trial due to a fear of infection, calibration of the system was carried out to fine-tune it to make it more accurate.
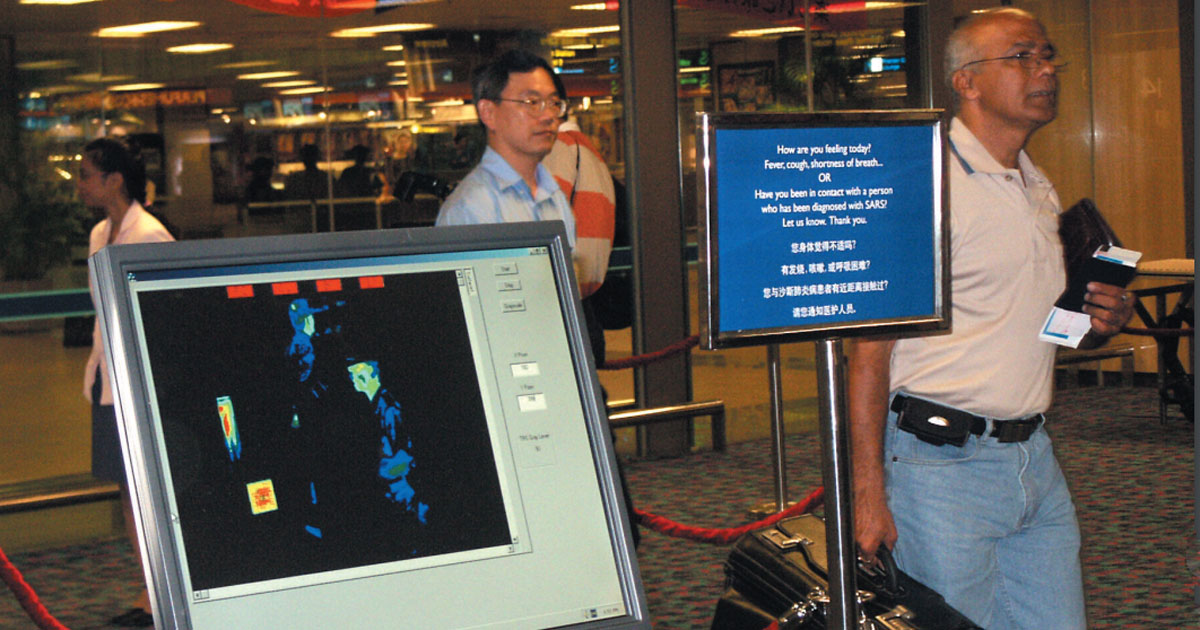
The mass fever screening prototype was then set up and tested at Changi Airport on passengers of selected flights.
These passengers still had their temperatures taken using physical thermometers to further cross-check and calibrate the system.
The mass fever screen device was declared operational at Changi Airport on April 11, 2003 -- exactly a week after they were rolled out for the first trial.
The result is the Infrared Fever Screening System (IFss).
Other tests were carried out at Alexandra Hospital and Tan Tock Seng Hospital subsequently.
An engineering feat
Some aspects of the fever screening system people might be unfamiliar with is that it was designed to detect relative temperature differences and was not regarded as an absolute temperature measurement tool.
It served as a sieve.
Anyone's facial temperature registered as 35.1°C and above would show up as red on the screen, indicating the person is febrile with a core body temperature that was likely higher than 38°C.
It was created as a trade-off between speed and accuracy -- a common engineering problem.
The first decision point is the detection of individuals with high skin temperatures.
The second decision point is the confirmation that the subject has an elevated body temperature using conventional clinical thermometers.
In other words, if the priority is to make sure that very few febrile people are missed, the threshold must be set lower -- at the expense of more false positives.
When first created, the false alarm rate was about 16 per cent.
But better to be safe than sorry.
Mass fever screening now
Moreover, adequate training of operators has become important for successful deployment of the system.
They will need to make judgement calls on borderline cases and that will depend largely on the experience and confidence of operators.
Once the system was deployed, they may be required to operate between 18 to 24 hours continuously.
This also means the devices require responsive technical support, as well as a logistics package including spares, preventive maintenance and corrective maintenance to ensure high equipment serviceability
Since then, the system has miniaturised: The latest real-time screening device simply uses a smartphone fitted with thermal and 3D laser cameras to detect the forehead temperature of individuals walking by.
If you like what you read, follow us on Facebook, Instagram, Twitter and Telegram to get the latest updates.